* Based on clinician-reported outcomes.
** Gordon, W. et al. “The Antimicrobial Efficacy of the Er,Cr:YSGG Laser with Radial Emitting Tips on Root Canal Dentin Walls Infected with e. Faecalis.” JADA 138, July (2007): 992–1002.
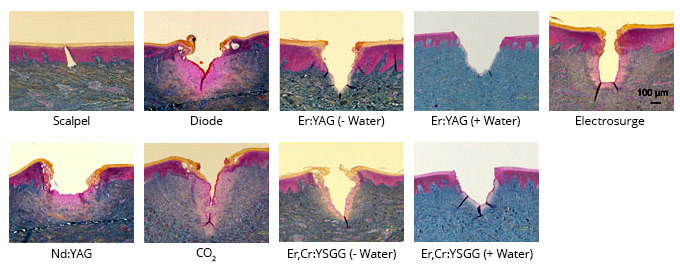
*** 1. Cercadillo-Ibarguren, I., et al. “Histologic Evaluation of Thermal Damage Produced on Soft Tissues by CO₂, Er,Cr:YSGG and Diode Lasers.” Medicina Oral Patología Oral y Cirugia Bucal 15, no. 6 (2010): e912–18. 2. Romeo, U., et al. “Histological in Vitro Evaluation of the Effects of Er:YAG Laser on Oral Soft Tissues.” Lasers in Medical Science 27, no. 4 (2012): 749–53.
† Christensen, Gordon J. “First Look: Solea CO2 Hard and Soft Tissue Laser.” CLINICIANS REPORT, Volume 8 Issue 4, April 2015, Pages 1, 3 & 4
1. Hossain, M. et al. “Analysis of Surface Roughness of Enamel and Dentin after Er,Cr:YSGG Laser Irradiation.” Journal of Clinical Laser Medicine & Surgery 19.6 (2001): 297–303.
2. Baygin, O. et al. “The Effect of Different Enamel Surface Treatments on the Microleakage of Fissure Sealants.” Lasers in Medical Science 27.1 (2012): 153–60.
3. Kilinc, E. et al. “Thermal Safety of Er:YAG and Er,Cr:YSGG Lasers in Hard Tissue Removal.” Photomedicine and Laser Surgery 27.4 (2009): 565–70.
4. Fried, D. et al. “Mechanism of Water Augmentation during IR Laser Ablation of Dental Enamel.” Lasers in Surgery and Medicine 31, no. 3 (2002): 186–93.
5. Vogel, A. and V. Venugopalan. “Mechanisms of Pulsed Laser Ablation of Biological Tissues.” Chemical Reviews 103, no. 2 (2003): 577–644.
6. Majaron, B. “Thermo-Mechanical Laser Ablation of Hard Dental Tissues: An Overview of Effects, Regimes, and Models.” SPIE 3593, January (1999): 184–95.
7. Türkün, M. et al. “Bactericidal Effect of Er,Cr:YSGG Laser on Streptococcus Mutans.” Dental Materials Journal 25.1 (2006): 81–6.